Written by Dr. Nicole M. Vienna
December 23, 2021
We detected that you're using an older version of Internet Explorer. please upgrade IE 11 or later
Alternatively, you can install and use these secure and newest browsers: Chrome | Firefox | Safari for MacOS | Edge for Windows
Written by Dr. Nicole M. Vienna
December 23, 2021
Contrary to popular belief, there is no single test or checklist for diagnosing ADHD. Indeed, it is a complex neurobehavioral diagnosis and often misdiagnosed. To that end, ADHD shares many symptoms with other disorders, such as PTSD, personality disorders, anxiety, bipolar disorder, and depression. This article will give you a brief overview of the ADHD criteria, adults and ADHD, a neuropsychological approach to ADHD, and ADHD’s interaction in juvenile delinquency.
According to the DSM-5, ADHD is considered a neurodevelopmental disorder because symptoms begin in the developmental period. Individuals with ADHD have a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with life functioning. Inattentive symptoms can include:
Hyperactivity-impulsivity symptoms can include:
In addition, symptoms must have been present prior to age 12, present in two or more settings, and cause clinically significant distress or interfere with daily life functioning (work, school, relationships, etc.). Last, the symptoms cannot be better described by another disorder such as depression, anxiety, or a personality disorder.
These symptoms can result in three different types of presentations:
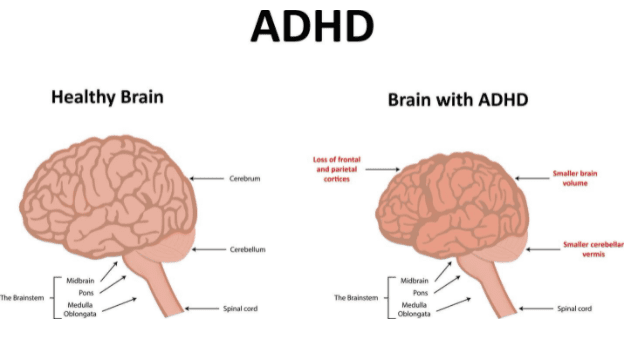
Numerous neuroimaging studies have found several morphological abnormalities in children’s brains with ADHD. Specifically, regional abnormalities include the reduced grey matter in the regions making up the frontostriatal circuits, atypical white matter volume in neural tracts (related to impaired communication between circuits), and cortical thinning. Still, over studies have found that ADHD is associated with reduced global brain volume. As such, ADHD is the result of complex abnormalities predominantly affecting the frontal lobes and other regions of the brain. In addition, it is important to note that genetic and adverse rearing association has been associated with reduced cortical volume in ADHD children. Thus, shining light on the role of parenting style and environmental influences on brain development.
While it has been thought to only exist in childhood, ADHD symptoms and impairments can persist into adulthood. Adult prevalence rates are estimated at 2.5% (Simon, et al. 2009). Still, other studies have found that over 10 million adults have ADHD.
Neuropsychologists are specifically trained in brain functioning, neuroanatomy, and brain-behavior relationships. Therefore, when assessing for ADHD, a neuropsychologist may use a variety of standardized cognitive tests and behavioral questionnaires. Depending on potential co-occurring issues, an ADHD evaluation can be very narrow-focused or broadly assessed to rule out or confirm cofounding problems. The tested cognitive domains can include intelligence, memory, learning, attention, problem-solving, organizational skills, and emotional regulation. Once the data is analyzed, the clinician will write a succinct report, including treatment recommendations to help improve daily life functioning.
Children with ADHD have impairments that can result in various problematic behaviors that can get them mixed into the juvenile justice system. For example, their difficulties paying attention in class, excessive talking and disruption, inability to sit still, being unable to not be distracted (inattention problems), not being able to stop internal thoughts (impulsivity), or being unable to stop acting upon distractions and/or thoughts (hyperactivity) can get them into trouble with their parents or school officials which then can lead them into truancy and eventually dropping out altogether. And if these symptoms continue to go untreated, these children may turn to drugs/alcohol to self-medicate unremitted symptoms, thereby increasing their risk of poor decision making and asocial behavior and coming in contact with the legal system.
Also, children with ADHD may have problems with self-talk (our ability to talk to ourselves), sense of time (in that time can seem to go by very slow or very fast), and shifting from plan A to Plan B. Lastly, they are more likely than their peers to struggle with separating emotion from fact, again, increasing their risk of asocial behavior and engaging in behavior that is not well thought out.
ADHD is a complex neurobehavioral diagnosis that shares overlapping symptoms with bipolar disorder, PTSD, anxiety, depression, and even some personality disorders. While most thought to exist in children, some studies have shown upwards of 10 million adults have ADHD. A neuropsychological evaluation can help assess executive functioning systems among other cognitive domains implicated in ADHD. This includes standardized cognitive paper-pencil testing as well as behavioral and symptom questionnaires. Untreated or mismanaged symptoms can lead to self-medicating with drugs or alcohol, thereby increasing their risk of asocial behavior, which is not well thought out.
If you would like to learn more about ADHD, contact our office to speak with Dr. Vienna. Call us at (626) 709-3494.